When something smells like a miracle, the internet crowd surfers start shouting. Autophagy — the cell’s process of breaking down damaged parts and recycling components — is legitimately exciting to researchers.
It’s implicated in cellular quality control, immune function, and possibly aging.
Table of Contents
ToggleThat combination of plausibility + complexity is a perfect breeding ground for extreme claims.
This article does three things:
- Explain what autophagy actually is in plain language.
- Tackle common myths (short claim + scientific reality).
- Draw evidence-based practical takeaways so you can use fasting and lifestyle tools safely and effectively.
I’ll explain technical terms in brackets when needed, avoid academic jargon, and be clear where evidence is solid versus still preliminary.

WHAT IS AUTOPHAGY? PLAIN-LANGUAGE, WITH A LITTLE BIOLOGY
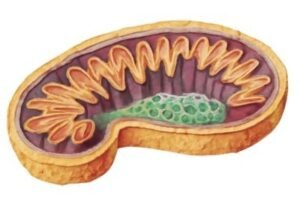
Autophagy (from Greek: auto = self, phagy = eating) is a cellular recycling program.
Cells package damaged proteins, old mitochondria (cellular batteries), and other waste into membrane-bound vesicles (called autophagosomes).
These then fuse with lysosomes (cellular “stomachs”) where enzymes break the contents down into building blocks that can be reused.
Why this matters:
- Keeps cells functioning well (less “junk” = better performance).
- Helps cells survive when nutrients are scarce by reusing internal components.
- Plays a role in immune surveillance (helps remove pathogens) and in removing damaged components that otherwise accumulate with age.
Important caveat: autophagy is not a single on/off switch.
It’s a family of related processes (macroautophagy, mitophagy — the selective removal of mitochondria — chaperone-mediated autophagy, etc.)
that operate in different tissues and respond to different signals.
Myth 1 — “AUTOPHAGY STARTS AT EXACTLY 16 HOURS” (or 24, 36, 72 hours)
Claim: There’s a precise, universal hour where autophagy begins.
Reality: Timing varies widely. Yes, autophagy increases during fasting, but there’s no single universal clock. The onset and magnitude depend on multiple factors:
- Metabolic state: People on a low-carb or ketogenic diet often enter ketosis (fat-burning) faster; this can accelerate metabolic signals that promote autophagy.
- Prior feeding: A high-carbohydrate meal delays the shift.
- Age and sex: Ageing cells may have a blunted autophagy response; hormonal differences may alter timing.
- Activity level: Exercise activates pathways that can synergize with fasting to trigger autophagy.
- Tissue differences: Autophagy in the liver may ramp sooner than in brain tissue.
Evidence summary: Animal studies (rodents) show robust autophagy induction at various fasting durations, but human data are limited and indirect (blood biomarkers, metabolic readouts).
Translating rodent hours to humans is not straightforward—rodents have faster metabolisms.
So, claiming a single hour threshold is misleading.
Practical takeaway: Use time ranges and signals, not a single timestamp. For many people, low-level autophagy-related processes begin in the 12–24-hour range, deepen after 24–48 hours, and are often pronounced by 48–72 hours — but individual variation is normal.
Myth 2 — “AUTOPHAGY = KETOSIS (they are the same thing)”
Claim: If you’re in ketosis (fat-burning), you’re doing autophagy; they are identical.
Reality: Ketosis and autophagy are related but distinct processes.
- Ketosis is a metabolic state where the liver produces ketone bodies from fatty acids to provide alternative fuel (beta-hydroxybutyrate, acetoacetate).
- Autophagy is the cellular recycling process described earlier.
They often occur together during fasting or low-carb diets because both are responses to nutrient scarcity and low insulin. However, one does not guarantee the other:
- You can be in ketosis (e.g., ketogenic diet) with variable autophagy depending on caloric intake and signaling pathways (mTOR activity, insulin levels, AMPK activation).
- Some interventions that trigger autophagy (e.g., certain exercise or pharmacologic agents) might not produce high blood ketones.
Evidence summary: Experiments show overlapping signaling—ketones can act as signaling molecules and may enhance autophagy in some contexts—but ketosis is not a direct measure of autophagy.
Practical takeaway: Don’t use blood ketone numbers alone as proof you’re achieving cellular cleanup. Ketones are useful markers of fat-burning, not autophagy per se.
Myth 3 — “AUTOPHAGY WILL CURE CANCER” (or prevent it completely)
Claim: Triggering autophagy through fasting will cure or prevent cancer.
Reality: Autophagy has a complex, context-dependent role in cancer:
- In some contexts, autophagy prevents cancer initiation by clearing damaged organelles and reducing inflammation.
- In established tumors, however, cancer cells can hijack autophagy to survive nutrient stress (including stress from therapies), making them more resistant.
Thus, autophagy can be both tumor-suppressive and tumor-promoting, depending on cancer type, stage, and genetic context.
Evidence summary: Preclinical studies show that blocking autophagy can make some tumors more sensitive to chemotherapy, while in other models inducing autophagy has preventive effects. Clinical applications are nuanced and under investigation.
Practical takeaway: Autophagy is not a stand-alone cancer cure. For people undergoing cancer treatment, fasting protocols should only be considered under oncologist supervision and as part of structured clinical research or careful medical guidance.
Myth 4 — “MORE AUTOPHAGY IS ALWAYS BETTER” (the ‘more-is-better’ fallacy)
Claim: The more autophagy you trigger, the healthier you’ll be.
Reality: Balance matters. Autophagy is protective up to a point; excessive or dysregulated autophagy, or autophagy triggered in the wrong context, can be harmful.
- During development or in certain diseases, excessive autophagy may contribute to cell death.
- In fragile or malnourished individuals, aggressive fasting can cause catabolism (breaking down needed tissue), electrolyte imbalances, and other problems.
Evidence summary: Most beneficial effects in models follow intermittent, controlled induction of autophagy, not chronic, unregulated induction. Homeostasis (balance) is key.
Practical takeaway: Aim for safe, repeatable protocols (e.g., intermittent fasting, occasional extended fasts with supervision) rather than extreme, frequent prolonged fasting without guidance.
Myth 5 — “AUTOPHAGY REVERSES AGING IN HUMANS” (overhyped longevity claims)
Claim: Turn on autophagy and you’ll reverse aging — human lifespan will be dramatically extended.
Reality: Autophagy is one of several biological processes associated with aging. Enhancing autophagy in animal models (yeast, worms, flies, mice) can extend lifespan and health span. But translating these findings into humans is not direct.
- Aging is multifactorial (genetics, telomeres, epigenetics, metabolic health, immune function). Autophagy modulation is a promising lever, but not a silver bullet.
- Human longevity trials are complex, long, and subject to confounders.
Evidence summary: Strong preclinical support, but limited direct evidence in humans that increased autophagy alone lengthens lifespan. That said, autophagy likely contributes to health span benefits seen with other interventions (caloric restriction, exercise, metabolic health).
Practical takeaway: Consider autophagy as part of a broader longevity strategy (sleep, exercise, diet quality, mental health), not the only focus.
Myth 6 — “YOU CAN MEASURE AUTOPHAGY EASILY AT HOME” (biomarker confusion)
Claim: A specific blood test or urine strip tells you exactly how much autophagy you have.
Reality: There is no simple, validated home test to quantify autophagy systemically in humans. Researchers use tissue biopsies, specialized imaging, or molecular markers (LC3, p62) measured in lab settings. Blood ketones, glucose, or insulin are indirect metabolic markers and do not measure autophagy.
Evidence summary: Most clinical studies infer autophagy indirectly (by measuring metabolic state, downstream effects, or by sampling tissue), but standardized, non-invasive human autophagy assays are not widely available.
Practical takeaway: Beware products or services promising “autophagy testing.” Use practical markers (weight trends, metabolic labs, clinical symptoms) and, if necessary, specialized clinical assessments under professional care.
Myth 7 — “AUTOPHAGY IS ONLY TRIGGERED BY FASTING” (single-trigger oversimplification)
Claim: Only fasting can trigger autophagy.
Reality: Autophagy responds to multiple stimuli:
- Fasting/caloric restriction is a strong trigger.
- Exercise, particularly vigorous or resistance training, can enhance autophagy in muscle.
- Certain pharmacologic agents and compounds (e.g., rapamycin — an mTOR inhibitor in research settings) modulate autophagy.
- Nutrient signaling (low amino acids, low glucose) influences autophagy.
- Intermittent hypoxia or stressors can also alter autophagy.
Evidence summary: A combination of lifestyle levers (fasting, exercise, sleep optimization, and good nutrition) likely yields the best outcomes for coordinated autophagy induction across tissues.
Practical takeaway: Use a multimodal approach: intermittent fasting + regular exercise + adequate sleep + nutrient-dense diet.
WHAT THE EVIDENCE DOES SUPPORT — STRONG AND MODERATE FINDINGS
Strong evidence
- Autophagy is an evolutionarily conserved cellular housekeeping mechanism, clearly demonstrated in many organisms.
- Fasting and caloric restriction robustly increase autophagy markers in animal models; many metabolic benefits (improved insulin sensitivity, reduced inflammation) relate to these changes.
- Exercise stimulates autophagy in muscle, contributing to improved metabolic health.
Moderate/Developing evidence
- In humans, fasting improves metabolic markers (insulin sensitivity, lipids) and likely activates autophagy indirectly; direct measures are harder to collect, but the metabolic milieu (low insulin, high AMPK activity) favors autophagy.
- Short-term fasting can improve inflammatory markers and cellular stress resilience.
- In some controlled settings, fasting around chemotherapy (under clinical supervision) shows promise for reducing side effects; but larger trials are ongoing.
Preliminary/cautious evidence
- Claims about autophagy curing or broadly preventing cancer are context-dependent and not universally supported.
- Longevity extension evidence in humans is suggestive but not conclusive.
Translating Evidence into Safe Practice — HOW TO “USE” AUTOPHAGY WISELY
If you want to harness autophagy safely and effectively, here’s an evidence-aligned approach:
Start with daily time-restricted feeding (TRF)
- Example: 14:10 or 16:8 (fast 14–16 hours daily, eat within an 8–10-hour window).
- Why: Sustainable, reduces daily insulin exposure, supports metabolic flexibility.
Add regular movement
- Resistance training and brisk walking stimulate autophagy in muscle and improve insulin sensitivity.
Occasional supervised extended fasts
- 24–72-hour fasts can deepen autophagy signals but should be attempted after adaptation and ideally with clinical guidance — especially for people with medical conditions.
Prioritize sleep and circadian alignment
- Poor sleep disrupts metabolic signaling; sleeping during the night and eating during daylight aligns autophagy and repair processes.
Nutrition quality in feeding windows
- Adequate protein, micronutrients, fiber, and healthy fats support repair and refeeding. Avoid extremes that cause nutritional deficiency.
Medical supervision if you have chronic disease
- Diabetes, pregnancy, eating disorders, or use of certain medications require medical input.
PRACTICAL EXAMPLES & COMMON PITFALLS
Example 1: Someone tries a 72-hour fast after years of grazing. Result: dizziness, severe hunger, and electrolyte disturbance.
- Lesson: Build up tolerance with daily TRF, hydrate, and consider electrolyte supplementation.
Example 2: A person uses “autophagy supplements” promising immediate benefits. Result: wasted money and potential side effects.
- Lesson: Skepticism is healthy—no supplement replaces the physiological signals from controlled fasting and exercise.
Example 3: A cancer patient reads that autophagy “will cure cancer” and stops chemotherapy. Result: dangerous delay in evidence-based care.
- Lesson: Do not abandon standard medical treatment based on oversimplified internet claims. Discuss adjunct fasting strategies only with your oncology team.
EMERGING FRONTIERS — WHERE RESEARCH IS HEADED
Research areas to watch:
- Selective autophagy modulation: Targeting specific autophagy pathways (e.g., mitophagy) to treat neurodegenerative diseases.
- Combining fasting with therapies: Using fasting or fasting-mimicking diets to sensitize tumors to chemotherapy under controlled conditions.
- Biomarkers development: Creating non-invasive, reliable markers of autophagy in humans (a major need).
- Personalized regimens: Determining which people benefit most from which fasting patterns based on genetics, microbiome, and metabolic phenotype.
All these are promising, but require rigorous clinical trials before broad clinical recommendations.
Frequently Asked Questions
Q: How long should I fast to “get autophagy”?
A: There’s no one-size-fits-all time. Low-level autophagy-related activity may begin in the 12–24-hour window; deeper effects commonly occur after 24–48 hours. Start with regular 14–16-hour daily fasts and progress carefully.
Q: Can I take supplements to trigger autophagy faster?
A: Some compounds (in laboratory settings) modulate autophagy, but there’s no safe, reliable home supplement validated to replace dietary and lifestyle measures. Focus on diet, exercise, sleep, and medically supervised interventions when needed.
Q: Is autophagy dangerous?
A: Not when induced responsibly. Risks occur with extreme fasting, electrolyte imbalance, untreated chronic disease, or in vulnerable populations. Supervision is advised for extended fasts.
Q: Does exercise trigger autophagy?
A: Yes — particularly in muscle. Combining regular training with fasting is synergistic for many people.
Q: How do I know it’s working?
A: Clinical benefits (better sleep, reduced inflammation, improved glucose control, increased energy) are practical signals. Direct measurement of autophagy remains a research tool.
Respect complexity; use simple, safe tools
Autophagy is genuinely fascinating and holds promise for improving health span and resilience. But the story is nuanced.
Animal studies provide proof of principle; human translation is underway but not yet definitive for many assertions you see online.
If you want to harness autophagy:
- Use time-tested, low-risk strategies: intermittent fasting, exercise, sleep, and quality nutrition.
- Avoid absolutist claims and quick-fix products.
- Seek professional guidance for extended fasting or if you have medical concerns.
Autophagy is not a myth — it’s real biology. But it’s also not magic.
The path to cellular repair is grounded in consistent, evidence-aligned lifestyle habits, occasional deeper protocols when appropriate, and sensible clinical oversight when needed.